INTRODUCTION 2019
The United Kingdom National Bariatric Surgery Registry
PUBLICATION OF SURGEON-LEVEL DATA IN THE PUBLIC DOMAIN FOR BARIATRIC SURGERY IN NHS ENGLAND
Summary
The NBSR Committee on behalf of the British Obesity and Metabolic Surgery Society presents the operative outcomes data for NHS patients having bariatric surgery for the three financial years 2012/13 to 2014/15 on http://nbsr.e-dendrite.com. These data add to and supersede the previous reported results for 2012/13 and 2013/14 due to the adoption of new definition of revision surgery and splitting of this into major and minor revisions. The main results are summarised in the table below. All NHS data are included and there were no non-contributing hospitals. The total number of hospitals includes private hospitals where these were used to provide additional capacity for the NHS bariatric units. The data shown are those of surgeons currently practising to our knowledge within the NHS and excludes recently retired surgeons.
Year |
Number of surgeons submitting data |
Number of hospitals |
Number of NBSR operations recorded * |
Number of primary operations |
Total number of revision operations (%) |
Number of major revisions |
Number of minor revisions |
2012/13 |
120 |
74 |
5,528 |
5,192 |
336 (6.1%) |
115 (2.1%) |
221 (4.0%) |
2013/14 |
139 |
69 |
5,729 |
5,297 |
432 (7.5%) |
167 (2.9%) |
265 (4.6%) |
2014/15 |
140 |
70 |
5,671 |
4,989 |
682 (12.0%) |
299 (5.3%) |
383 (6.7%) |
Total |
- |
- |
16,928 |
15,478 |
1,450 (8.5%) |
581 (3.4%) |
869 (5.1%) |
Year |
Number of NBSR primary operations and major revisions |
HES recorded data (NBSR case ascertainment %) |
Recorded in-hospital mortality (%) ** |
HES recorded in-hospital mortality (%) |
ONS recorded 30-day mortality (%) |
2012/13 |
5,307 |
6,168 (85.6%) |
5 |
4 (0.06%) |
14 (0.22%) |
2013/14 |
5,464 |
5,612 (97.3%) |
5 |
3 (0.05%) |
5 (0.08%) |
2014/15 |
5,288 |
5,425 (97.5%) |
2 |
0 (0.0%) |
4 (0.07%) |
Total |
16,059 |
17,205 (93.3%) |
12 (0.08%) |
7 (0.04%) |
23 (0.13%) |
* These data include all primary and revision surgery, without subdividing revision surgery into major and minor. Therefore the numbers include re-operations for complications of the primary procedure (which may not be detected as bariatric operations by HES) as well as conversions to another bariatric procedure.
** The NBSR mortality data we report are in-hospital deaths and exclude patients who may be readmitted and die due to a complication of surgery within 30 days. The data are adjusted compared to previously reported as entries on the registry have been changed/edited by contributing surgeons. The two deaths reported as in-hospital deaths in 2014/15 were patients who went home and were readmitted and died within 30 days; however they were recorded as in-hospital deaths by the structure of the registry. Twelve consultants in different hospitals had one death each and none was a potential statistical outlier.
A future version of the dataset (planned for 2016) will enable deaths to be distinguished between happening either in-hospital or after readmission. Due to the Data Protection Act we are not able to ascertain whether the 30-day deaths recorded by the ONS included these two patients.
Overall for the 3 years, primary surgery:
- The average patient body mass index (BMI) was 49.8 kg/m2 and the average weight was 138.3kg, indicating that the patients were twice the ideal weight for their height
- 74.4% patients were female
- The average number of obesity-related diseases for each patient, for example type 2 diabetes, hypertension, sleep apnoea, functional impairment and arthritis was 3.57
- There were 12 recorded deaths for an in-hospital mortality rate of 0.08%, equivalent to a survival rate of 99.9%
- The average length of hospital stay for all operations was 2.7 days
- There were no potential statistical outliers for mortality or length of stay
The data presented here for 2014/15 corroborate the high levels of obesity-related disease combined with low mortality and short length of stay for bariatric surgery published in the 2013 and 2014 Bariatric Consultant Outcomes Publications 1, 2. The ONS data indicate that the 30-day mortality rate continued to fall compared to the 2 years 2012/14 when it was 0.17%.
In-hospital and 30-day survival from bariatric surgery continues to improve and be at least as good if not better than many common laparoscopic gastrointestinal procedures.
Richard Welbourn (Chair), Simon Dexter, Ian Finlay, James Hopkins, Omar Khan, Marcus Reddy, Peter Sedman, Peter Small, Shaw Somers
NBSR Committee
25th March 2016
BACKGROUND
The first round of Consultant Outcomes Publication in 10 specialties, including bariatric surgery, in summer 2013, followed a call for a culture of openness, transparency and candour from the Francis Report (2013) that dealt with the events leading up to the Mid Staffordshire enquiry 3. The National Bariatric Surgery Registry (NBSR) published its individual consultant outcomes data for 2012/13 on 2nd July 2013 and for 2013/14 on 30th October 2014 for surgeons in the NHS in England 1, 2. As for 2013/14 the 2014/15 report includes the ability to search for results for each hospital.
For the next iteration of the process we are invited by Sir Bruce Keogh to highlight examples of good practice (positive outliers) as well as publishing the names of potential negative statistical outliers. We are also asked to publish more outcomes for 2014/15 than in the previous years. As participation in the NBSR is a mandatory part of provider contracts, this year the NBSR Committee:
- Publishes the names of the hospitals whose total patient records were >10% fewer than they should be according to HES
- Adds the percentage of initial patient records that are ‘green for complete’
- Sub-divides revision surgery into major and minor, so as to highlight the work of those who take on higher risk major revisions.
We are well aware of the lack of audit back up in many units and the first two are intended to support surgeons in their discussions locally. Outcome 2, for the first time in NBSR reporting, produces potential negative (and positive) outliers.
DETAILED OUTCOMES PUBLISHED FOR 2014/15
In 2013/14 we reported additional outcomes and do so again for the 2014/15 round. The new 2014/15 outcomes are:
- The names of hospitals whose NBSR entries are more than 10% fewer than they should be according to Hospital Episodes Statistics (HES) (poor case ascertainment)
- Data completion rates for the initial in-patient record according to the proportion of records that are ‘green for complete’ for each surgeon
- Reporting of revisional surgery rates according to major and minor, expressed as % of workload of each surgeon.
NOTES ON THESE OUTCOMES
1. Case ascertainment vs Hospital Episodes Statistics (HES)
We reprint here the text from the 2013/14 report where we call for hospitals to provide sufficient administrative support to help their surgeons and bariatric teams with data entry:
‘‘It is evident that most NHS bariatric units still don’t have sufficient administrative support to ensure completeness of data entry and internal validation. Although the NBSR became mandatory for NHS providers from 1st April 2013, we remind hospital Trusts of their obligation to:
- Verify and facilitate consultant and hospital-level engagement with national clinical audit; including providing resource for data validation
- Respond to audit provider requests to check data accuracy and notification of outlying data
- Work with clinicians and audit providers to use audit data ‘real-time’ for quality improvement
- Promote the value of clinical audit across all work streams, not just those involved with COP 4
Our view remains that it is insufficient to rely on individual clinicians alone to ensure there are no missing records, incomplete records or inaccurate data entry and thus possible under-reporting.’’
For the 2014/15 report we report the names of the 7 hospitals whose records were more than 10% fewer than they should have been according to HES, excluding hospitals where there are 10 or fewer patients apparently missing:
- Castle Hill Hospital, Cottingham
- Dewsbury & District Hospital, West Yorkshire
- Doncaster Royal Infirmary
- King's College Hospital, London
- Walsall Manor Hospital
- North Tyneside General Hospital, South Shields
- Royal Derby Hospital
For the 2013/14 report we took 2 data cuts, in July and September 2014. Seventeen hospitals were identified as having more than 10% fewer patient records submitted to the NBSR than recorded in HES. Therefore the 2014/15 data represent an improvement overall.
Letters according to the policy on the BOMSS website are being sent to these hospitals to remind them of the requirement to provide sufficient administrative support for data entry. It is possible that individual hospital coding issues are the reason for the apparent differences, and these need assessing locally. Although mandated in the NHS provider contracts, the NBSR committee has no further role other than pointing out the apparent lack of case input.
In addition to naming, and sending letters to, hospitals with more than 10% fewer patient records than indicated by HES we took an executive decision to exclude hospitals from this category if there were 10 or fewer cases missing. Four hospitals with small operative numbers had >10% missing and 10 or fewer cases missing and so were not named.
Overall for the 3 years, case ascertainment, that is the cases recorded into the NBSR expressed as a proportion of the total, has improved from 85.6% to 97.5%, calculated as the number of primary operations plus major revisions divided by the total operations in HES (which does not include 30-day reoperations).
The r2 value for HES vs NBSR entries is 0.95, indicating close overall correlation between the HES codes we are using and caseload entered into the NBSR, correcting for one hospital that had 304 patient according to HES, with only 48 entered into the NBSR, and correcting for another on two sites where 56 patients recorded in HES were done at the other hospital. Without these corrections the r2 value is 0.85.
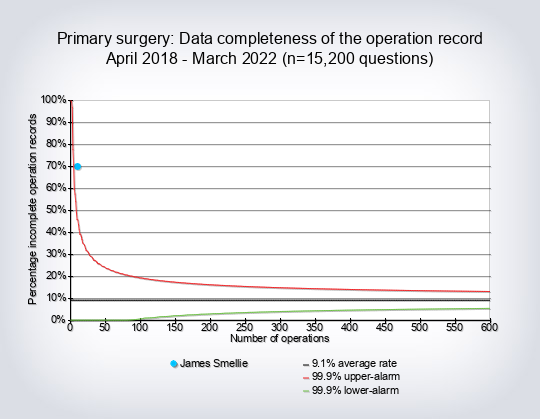
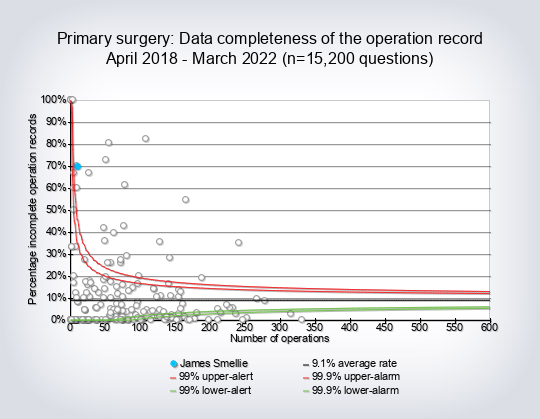
2. Data completion rates – initial record ‘green for complete’
The First NBSR Report details the data fields that need to be completed to make the record go green 5. If one or more field is missing the data record will remain yellow for incomplete. The fields are:
Initial information
- Weight
- Height
- Hospital name
- Funding Category
Baseline comorbidity
- ASA grade
- Type 2 Diabetes and duration (where applicable)
- Hypertension
- Cardiovascular
- Sleep apnoea
- Asthma
- Functional Status
- Known risk factors for pulmonary embolus
Operation Record
- Type Of Operation (Primary, Revision or Planned Second Stage)
- Operative approach (Laparoscopic, Lap converted to Open, Open, Endoscopic)
- Operation (select relevant choice)
- For Revisions Prior Operation Type (where applicable)
Post-op course and discharge
- Cardiovascular complications
- Other complications
- Discharge date
- Discharged destination
Twenty-four surgeons were potential negative outliers for data completion at the 99.9% alarm level and will be sent letters as per the policy published in 2013 on the BOMSS website 6. We were contacted by one hospital that has a local version of the database and does not have the same green colour change to indicate that the record is complete (as compared to ‘yellow for incomplete’). Since the timescales involved and uncertainty about funding for the process made it possible for there to be one data cut only, on 28th November 2015, there was no opportunity to correct that hospital’s surgeons’ data for the present report, ie to ensure that all the necessary data were completed in a form that could be uploaded. However a future data cut in around October 2016 for the 2014/15 publication will show all updated records to that point, for all contributing surgeons.
Seventy-three surgeons were positive outliers at the 99.9% level ie had near-complete or complete data completion.
3. Primary and Revision surgery are here defined as
- Primary surgery: the first bariatric operation
- Minor revision: all operations for later complications of surgery, which may or may not involve laparoscopy or laparotomy, and includes band port and band removal procedures
- Major revision: where one operation is converted to another bariatric operation, including planned second stage procedures
Minor revision surgery includes reoperations for complications of all bariatric procedures, ranging from more minor reoperations on for instance a subcutaneous gastric band port to more major reoperations for complications eg a leak from or stricture in a staple line, or bleed from a gastric bypass or sleeve gastrectomy. The definition also includes re-operations for internal hernia (twisted bowel) that can occur after some types of surgery. Operations such as cholecystectomy are not recorded as revisions with this definition.
Major revision surgery includes an operation for instance where a vertical banded gastroplasty (now obsolete) is converted to a gastric bypass, or a band procedure is added to a gastric bypass. Experienced surgeons may be more likely to perform more major revisional surgery, compared to younger, newly appointed consultants.
Future reports may sub-divide ‘Minor revision surgery’ into local procedures not involving laparoscopy/laparotomy, and more invasive procedures that involve laparoscopy/laparotomy since the current definition encompasses a wide range of invasiveness. Future reports may also include post-operative complications occurring within or after 30 days of the index procedure.
MORTALITY VALIDATION FROM HES
We use the same methodology as for 2012/13 and 2013/14 and this is specified in the previous reports 1, 2. The in-hospital and 30-day mortality rates after surgery continue to fall, with no in-hospital deaths reported for 2014/15. In particular, the data checked against the Office of National Statistics Births, Marriages and Deaths Register indicate that there were 23 deaths in 17,205 patients (0.13%) over the three years 2012/15, a decrease from the rate of 0.17% reported cumulatively to 2013/14 2.
The definition of in-hospital death used for the NBSR and HES reporting is a death that occurs during the initial hospital stay before discharge. There were no recorded in-hospital deaths in HES and four 30-day deaths, checked against Office of National Statistics data. There were 2 recorded in-hospital deaths in the NBSR. Further local investigation of these indicated that the patients had been re-admitted to hospital after discharge and had subsequently died within 30 days. The rules regarding publication of small numbers do not allow us to investigate further but we assume that they were in the 30-day recorded ONS deaths.
The recording of the 2 NBSR deaths as occurring in-hospital may be anomalous due to the precise way that the deaths were entered onto the database, where the analysis programme fails to discern that a discharge and readmission has happened before the death occurs. It is reassuring however that the surgeons are making it very clear that a death is recorded and that their mortality is in the public domain. In addition, there is a new policy concerning non-submission of mortality data on the BOMSS website http://www.bomss.org.uk/wp-content/uploads/2014/04/NBSR-Policy-for-Managing-Non-Contribution-of-Patient-Data-March-2015.pdf.
We reproduce here a paragraph regarding estimating mortality after 30 days from the 2013/14 report 2:
‘‘The current analyses of mortality do not extend beyond 30 days. Although it is theoretically possible to perform a 6-month analysis via the ONS of deaths after surgery for instance from ongoing complications, we do not have the resource to do this. In addition, mortality would have to be checked against individual death certificates, which is beyond our administrative and logistical capacity. Also, the analysis would have to take into account the background rate of mortality in the population unconnected with surgery and therefore the results would be even more difficult to interpret.’’
We are fully supportive of the practices, as far as we know the details, of the 12 surgeons from different hospitals who each reported one death in the analysis period. None was a statistical outlier. The NBSR data and the various HES analyses are entirely equivalent to a US benchmark, the American College of Surgeons Bariatric Surgery Center Network, where the published mortality rate was 0.12% (35 out of 28,616) for patients operated from 2007-10 7.
OTHER OUTCOMES REPORTED
These are:
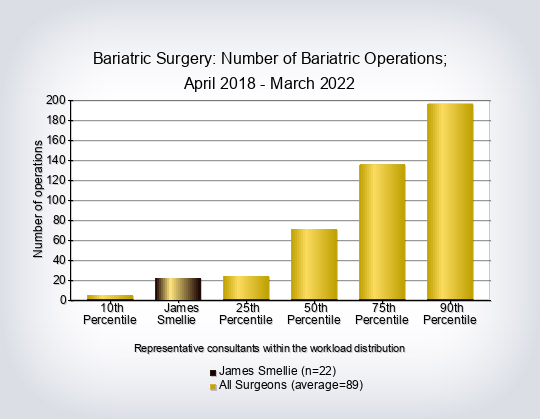
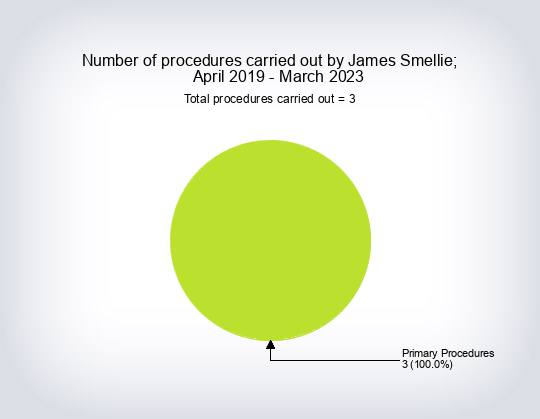
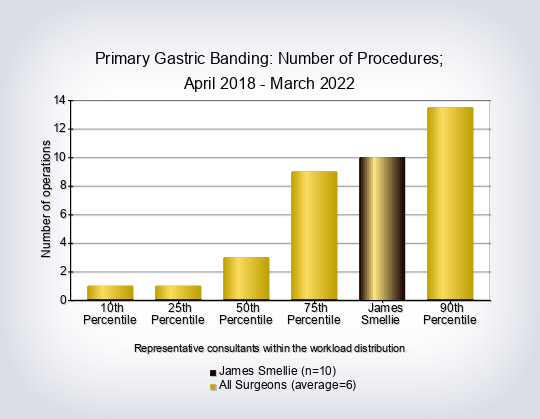
- Consultant workload for primary and revision operations excluding gastric balloon placement
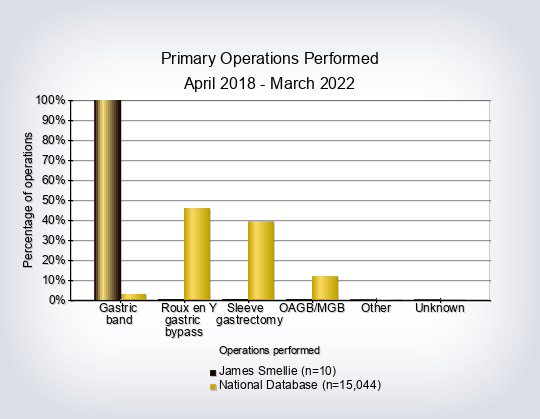
- Operation split by consultant
- BMI on entry into the weight loss programme
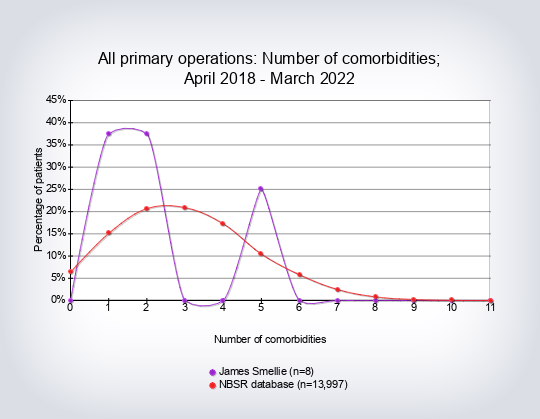
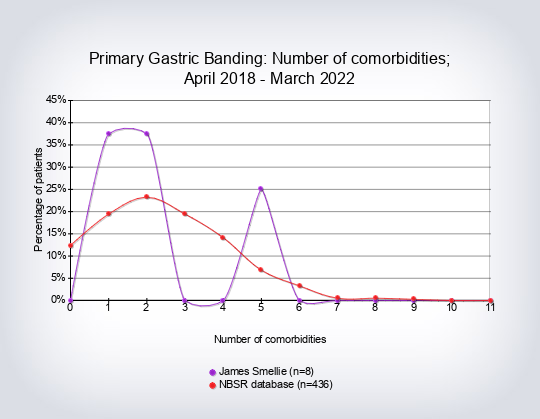
- Co-morbidity count per type of operation (number of co-morbidities recorded per patient)
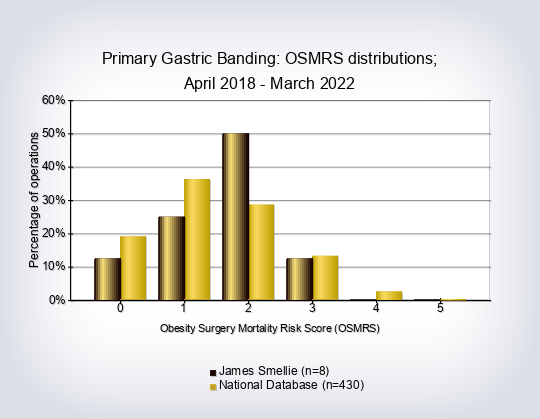
- Obesity-Surgery Mortality Risk Score (OS-MRS) and class per operations and overall per consultant
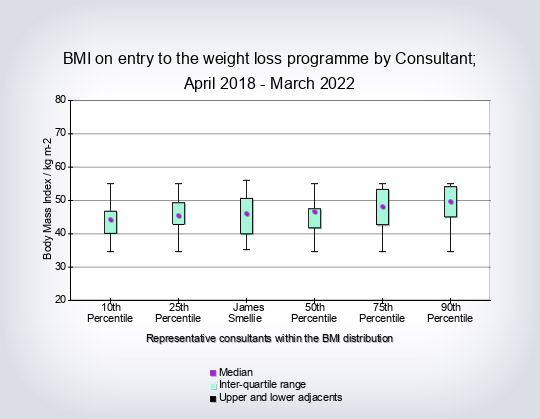
- Initial BMI overall per consultant (box and whiskers)
- Length of stay for primary procedures compared to the rest per consultant
- In-hospital mortality, described as survival
The co-morbidity count was taken from the NBSR dataset of co-morbidities:
- Type 2 diabetes
- Hypertension on treatment
- Dyslipidaemia
- Atherosclerosis (includes angina, MI, CABG, stroke, claudication)
- Sleep apnoea
- Asthma
- Functional status (presence of comorbidity defined as unable to climb 3 flights of stairs without resting)
- Back or leg pain from arthritis
- GORD
- Liver disease (suspected NAFLD or worse)
- Poly-cystic ovarian syndrome (female patients only)
- Depression (clinically significant depression as a reason for bariatric surgery)
The Obesity Surgery-Mortality Risk Score is the only validated measure of operative risk for patients undergoing bariatric surgery 8. A point is added for each of the following risk factors that are present, up to a maximum of 5 points: age at surgery ≥45 years, BMI ≥50 kg m2, male gender, recorded hypertension, one or more known risk factors for deep vein thrombosis (DVT) / pulmonary embolism (PE). Using the resultant score, complication & mortality rates can be risk-adjusted; the higher the score/group, the greater the risk of surgery. Patients can be stratified for risk according to how many of these risk factors are present. It is normal practice to refer to the calculated scores in three groups:
Group A (0-1 points)
Group B (2-3 points)
Group C (4-5 points)
We worked with the Quality Outcomes Research Unit in Birmingham University (QUORU) to analyse the HES data, and using a refined set of OPCS4 codes were able to estimate the mortality for primary bariatric surgery for the 3 years April 2012 – March 2015 previously highlighted (D McNulty, D Pagano, P Small, R Welbourn unpublished). Due to time limitations we were not able to analyse HES data for any other potential outcome.
PRESENTATION OF RESULTS
Patients are now able to search for hospitals by geography using an added map function and postcode. See the Frequently Asked Questions section on how to interpret this. As before, we present data for each outcome variable either as graphs, bar charts or box and whiskers graphs. Comments are included interpreting the results.
Additional notes:
We were contacted by Sunderland Royal Hospital where intra-gastric balloon data are collected on a different system and are not currently submitted to in the NBSR. Also, a substantial proportion of gastric bypasses in Sunderland are constructed using a loop technique, which it is not possible to record in the NBSR. A loop gastric bypass page is planned for Version 2 of the NBSR to accommodate this changing practice. These differences accounted for the observed discrepancy in their NBSR numbers vs HES.
INTERPRETATION OF RESULTS
We believe the 3-year data for 2012/15 are a correct representation of surgeon and hospital volume, baseline BMI, degree of baseline obesity-related disease, type of operation, mortality and length of stay.
NBSR Committee, 25th March 2016
Contact details
The NBSR administrators Sarvjit Wünsch or Nichola Coates are contactable by email
or
, telephone 0207 869 6941 or post to The National Bariatric Surgery Registry, The Royal College of Surgeons of England, 35-43 Lincoln’s Inn Fields, London WC2A 3PE.
NATIONAL BARIATRIC SURGERY REGISTRY BOOK REPORTS
So far almost 50,000 individual patient records have been added since its inception in January 2009 and the First NBSR Report of aggregated operative and disease-related outcomes was published in April 2011 9. A Second NBSR Report of aggregated outcomes in 18,000 patients over 3 years was published in November 2014 10.
References
1.
Bariatric Surgeon-Level Outcomes Data 2013.
http://www.bomss.org.uk/wp-content/uploads/2014/04/Bariatric-Surgeon-Level-Outcomes-Data-Report-2-July-2013.pdf
2.
The UK NBSR. Publication of surgeon-level data in the public domain for bariatric surgery in NHS England.
http://www.bomss.org.uk/wp-content/uploads/2014/10/Bariatric_Surgery_Consultant_Outcomes_Publication_30_October_2014.pdf
3.
The Francis Report 2013 Executive Summary
http://www.midstaffspublicinquiry.com/sites/default/files/report/Executive%20summary.pdf
4.
HQIP Consultant Outcomes Publication. Manual for Stakeholders Version 3.0 August 2014.
5.
NBSR User Guide Summary July 09.pdf.
http://cl1.n3-dendrite.com/csp/bariatric/intellect/DocumentManagement.csp
6.
NBSR Policy for Identification of Potential Outliers. June 2013.
http://www.bomss.org.uk/wp-content/uploads/2014/04/NBSR-Policy-foridentification- of-potential-outliers-June-2013.pdf
7.
Hutter MM, Schirmer BD, Jones DB et al. First Report from the American College of Surgeons Bariatric Surgery Center Network Laparoscopic Sleeve Gastrectomy has Morbidity and Effectiveness Positioned Between the Band and the Bypass. Ann Surg 2011; 254: 410–422.
8.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surgery for Obesity and Related Diseases. 2007; 3(2): 134-40.
9.
First NBSR Report April 2011.
http://www.nbsr.org.uk/
10.
Welbourn R, Sareela A, Small P et al. National bariatric surgery registry: second report. 2014
http://cl1.n3-dendrite.com/csp/bariatric/cdb/BAR/upload/2nd%20NBSR%20Report%202014.pdf. ISBN 978-0-9568154-8-4.